In 2007 when two people got talking over lunch in a hospital canteen in Springfield, Massachusetts, little did they know where the conversation would lead them. The topic under discussion was surgeon Dr Philip Stoddard’s frustration with the limited and invasive options available to treat babies before surgery to repair cleft palates. He had an inkling that computer-aided design could be the key to improving the process for affected children.
Listening to Stoddard’s ideas was Beth Roscoe, a medical engineer and prosthetist working at the hospital, who had experience in computer-aided design and manufacturing. Roscoe believed she could help and suggested designing and tailor-making a set of plastic appliances that could fit over a child’s gums, similar to a retainer, for use in the weeks before surgery. The appliances could be made using laser scanning, reverse engineering and rapid prototyping.
A year later the pair’s idea became a reality as a child underwent pre-surgical treatment for cleft palate at the hospital using the appliances for the first time.
One in every 700 children born in the UK has some degree of clefting in the lip or palate, or both, making it the most common facial birth defect. It is caused when separate parts of the face do not join up properly during development in the womb, leaving a gap in the upper lip and roof of the mouth.
Children born with a wide cleft of their palate benefit from treatment to narrow the gap before surgery to repair the problem. Pretreating the cleft makes the operation to close the gap simpler and reduces tension on the lip scar, as the tissue is stretched over a smaller area. This gives better results for the child.
There are two pre-surgical techniques currently used to shrink wide clefts, but both have limitations. One involves surgery to pin an appliance to the roof of the mouth when the baby is one month old. The operation is done under anaesthesia, which carries risks. Once in place, the child’s mother tightens the device by turning a small screw every day. Not only is this treatment invasive, but some doctors say it inhibits growth of the jaw.
The other technique uses a plastic device that is fitted non-surgically to the roof of the mouth. Every week it is removed and reshaped manually by an orthodontist. Weekly visits to a cleft clinic can be time consuming and expensive for families that do not live nearby and the results can vary, depending on the skill of the orthodontist.
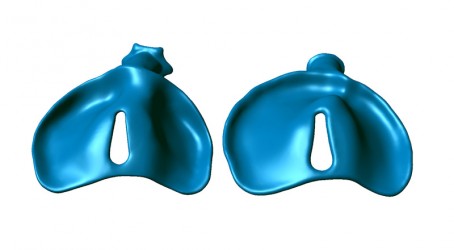
Roscoe and Stoddard’s technique uses a series of 12-15 nylon appliances that are changed weekly by the child’s doctor or mother. Each appliance in the series is slightly different from the previous one and they work by gradually moulding the roof of the mouth. With each week the two sides of the cleft become about 0.5mm closer, and over time this reduces the severity of the cleft. Roscoe explains: “It has been very well received because it is easy to administer, it’s not invasive, and it gets the desired result for the surgeon.”

The process begins with a surgeon taking an impression of the child’s gums. From the impression, a plaster positive mould is made and sent to Roscoe. She puts the mould into a scanner that runs a laser beam over the surface to read the dimensions of the roof of the child’s mouth. It does this by measuring the distances between different sections of the mould to create 200,000 3D points in space that represent the surface of the mould.
This data is then manipulated in the reverse-engineering software Geomagic to create a 3D model of the upper surface of the mouth. Next Roscoe uses mathematical models to predict the child’s jaw growth and work out how the palate and gums should be positioned by the time of surgery. This forms the digital blueprint for the final appliance in the series.
Taking the first and last models together, Roscoe can work out how many weeks will be needed to narrow the gap sufficiently for the surgeon. Using a 3D interpolation process she creates a digital plan of each of the appliances that will be needed from the start to the end of the treatment.
Roscoe explains: “I now have the surfaces of each palate shape, but it’s just a zero thickness representation of the shape. So I have to thicken it to create the digital model of the appliance.” Once the digital models are complete, the data is moved into a rapid prototyping machine, which manufactures the appliances using selective laser sintering.
The appliances must be very specific shapes to fit well in each child’s mouth, which rules out other manufacturing techniques, such as CNC milling, says Roscoe. “Injection moulding would be impractical. There is no alternative way to make an unusually shaped object from a digital file,” she adds.
In the four years since Roscoe and Stoddard first met in the canteen, six children have undergone the procedure. Increasing interest in the product has driven Roscoe to set up her own business, Custom Medical Components, to supply doctors around the US who want to use the technique. “I’m working on a baby from New Jersey now, so they can be anywhere,” she says. “As long as they can get to Federal Express.”
The company has partnered with a local manufacturing firm to produce the appliances. The design, manufacture and shipping of the devices takes about two weeks from the arrival of a child’s mouth mould, provided the initial design proofs are accepted by his or her doctor.
So far, too few children have undergone the procedure to enable a proper comparison of the results of the new technique with existing treatment methods. But initial results are promising. “I really believe that this is the best approach for the child. The cost is less than other methods,” says Roscoe. “I hope that in time it will catch on. It could benefit thousands of children.”
Roscoe has in mind several other medical applications that could use similar technology, but they remain under wraps for the time being.
- Do you think this treatment method has great potential? Tell us what you think by commenting below.