COVID-19 Section 5: Transmission and face masks
Introduction: face masks: a barrier to COVID-19
This chapter provides an insight on the use of face masks during a pandemic and how face masks can help curb the spread of various air or aerosol-borne infectious diseases.
Face masks, although a personal protective equipment (PPE) by function, have been shown to be one of the effective measures to help in stopping the spread of the pandemic when the majority of the population adopts it early on. This chapter will discuss the various face masks available to the general public and their efficacy along with the key issues and concerns regarding face masks.
Airborne transmissions can transmit small particulates through the air over time and distance. Airborne transmissions are usually distinct from transmission by respiratory droplets. Respiratory droplets are droplet particles greater than 5-10 μm in diameter whereas droplets less than 5 μm are referred to as droplet nuclei. Development of effective control measures against aerosol or airborne transmission of infections with various outbreaks like Severe Acute Respiratory Syndrome (SARS), human avian influenza A (H5N1), pandemic influenza A (H1N1/2009), and ongoing COVID-19 have become important. [1]
Transmission of infectious agents may occur via short-range, large-droplet aerosols and long-range, smaller, airborne droplet nuclei as shown in Figure 1. [2]
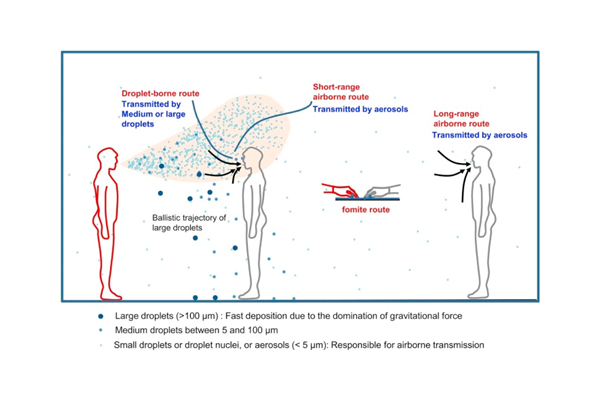
Figure 1. Illustration of different transmission routes of airborne and aerosol infections (Credit: Elsevier COVID-19 resource centre. [3]
From the experience gained in response to SARS in Southeast Asia, wearing face masks can help prevent spreading or breathing in infectious droplets to a certain degree and should be applied together with other risk control measures, such as hand hygiene, social distancing, ventilation control, and vaccination, to make a significant contribution to the prevention of COVID-19 [2].
Purpose of face masks
In general, face masks serve several purposes; they help reduce the amount of, as well as slowing down the speed of, droplet or aerosol breathe out or sneeze from an infected person to the environment, or reduce the amount of virus-contaminated air breathing in by an uninfected person. Face masks can also reduce the possibility of people touching their mouth and nose with contaminated hands or other objects.
Figure 2 shows the probability of a person being affected by aerosol or airborne virus in different scenarios. The probability greatly reduces when both individuals wear face masks. Face masks are mainly used to contain the spread of the virus from the wearer to others. One common misunderstanding is to assume face masks are mainly used to protect the wearers against contacting the virus. Depending on the application and type of masks, most face masks available in the market are designed to protect others against infection from the wearer.
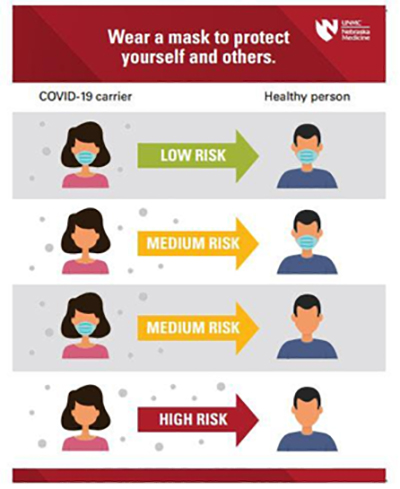
Figure 2. Transmission risk related to wearing masks
Cloth masks

Figure 3. Cloth masks
In circumstances where there is a limited supply of surgical masks, cloth masks can be an alternative for use in public. Cloth masks are defined as masks made of cloth or any other fabric such as cotton, gauze, silk, or muslin as shown in Figure 3. The filtration effectiveness of cloth masks is lower than that of surgical masks or respirators, but it can provide a certain degree of protection if it is designed to fit around the face and made water-resistant [6,7]. Some cloth masks allow a filtering layer that can enhance the protection against transmission. Since there is no specific technical standard or specifications to most of these cloth masks, they can only be treated as a contingency in shortage of a better mask and should not be viewed as an alternative to a better mask due to their style and colourful designs.
Few researchers point out that cloth masks made of tightly woven with 100% cotton material are relatively better than other cloth masks. A reason for this could be that the natural structure of cotton tends to have a more three-dimensional structure than synthetic fibers which eventually creates more blocks when the particles enter. Although masks with multiple layers are deemed to be more effective in blocking small particles, fabric, breathability and fit should also be kept in mind while choosing or making a mask [17].
UK researchers show that “hybrid” masks combining two layers of 600-thread-count cotton with materials like silk, chiffon, or flannel had a considerable effect in filtering small particles (about 80 percent) and large particles (more than 90 percent). Findings showed that combination of cotton and chiffon offered the most protection followed by cotton and flannel, cotton and silk, and four layers of natural silk. Recommendations from World Health Organisation (WHO) also state that fabric masks could have three layers: an inner layer which absorbs, a middle layer which filters, and an outer layer made from a non-absorbent material like polyester [18].
As per the BSI Guide, in the light of current covid scenario, WHO recommends a minimum of FFP2 (94% Filtering Efficiency) for offering protection. As different governments follow different approaches, BSI recommends that government should take a step up to identify the level of protection a face covering can provide and educate its population regarding the same. [21]
Copper mask
Copper masks are masks infused with a copper metal mesh layer. Copper oxide is known to display antiviral properties. Research shows that copper oxide impregnated face masks may filter above 99.85% of aerosolized viruses when exposed to the H1N1 virus and avian influenza virus (H9N2) under simulated breathing conditions [9]. Another important finding from the research was that no infectious viral titres were recovered from the copper oxide masks within 30 minutes. A cloth mask embedded with a copper mesh filter can significantly increase its efficacy and can be a viable alternative to a better mask unless being exposed to an environment that requires surgical masks [9].
Impregnation of copper oxide into protective face masks enables them with potent anti-influenza biocidal properties without making any change to their physical barrier properties. This will assist in significantly reducing the risk of hand and environmental contamination and hence subsequent infection due to improper handling and disposal of the masks. Several tests carried out show that the amount of copper eluted to air from test mask in a time period of 5 hours under simulated breathing conditions was 0.467±0.47 pg, which is far below the respiratory copper permissible exposure limit (PEL) set by USA Occupational Safety and Health Administration (OSHA) [9a]. The outer layers of the masks which contain copper oxide particles also did not cause any skin sensitization or skin irritation.
Mass distribution of copper masks was done in Hong Kong around the month of May. CuMask+™, developed by The Hong Kong Research Institute of Textiles and Apparel (HKIRTA) consists of six layers with two layers specially made with small quantities of copper as shown in Figure 6. This is capable of deactivating bacteria, common viruses, and other harmful substances. CuMask+™ complies with the American Society for Testing and Materials (ASTM) standards for particle filtration efficiency, bacterial filtration efficiency, resistance to penetration by synthetic blood, flammability, and pressure resistance [9].
Surgical masks
A surgical mask, also known as a medical face mask, is used by health professionals during healthcare procedures. These masks are designed to prevent infections in patients and personnel treating them by catching bacteria shed in liquid droplets and aerosols from the wearer's mouth and nose. An FDA-approved surgical mask is made from thin, disposable material as shown in Figure 4. Surgical masks are classified into two types – (1) which is used by patients and other persons to reduce risk of infection, and (2) which is used by healthcare professionals (which can also be splash resistant).
Surgical masks are made of nonwoven fabric created using a melt blowing process. These masks are disposable, loose-fitting masks. A metal strip at the top of the mask can be formed around the nose of the user [8]. These are designed for single use only and should be disposed of after use. These masks must be removed and replaced with another one when they become moist.
Different standardised tests are conducted to ensure performing properties are validated like Bacterial or Viral Filtration Efficiency (BFE/VFE), Differential Pressure, Flammability test, Particle Filtration Efficiency, and Synthetic Blood Fluid penetration resistance. Appendix 1 shows the details and the different levels of surgical face masks.

Figure 4. Surgical mask
N95 respirators
N95 respirators are respiratory protective devices that are engineered to achieve a very close facial fit and efficient filtration of airborne particles as shown in Figure 5. They are made of a material that filters most of the particles from the air when it passes through the face mask – as long as the respirator is correctly fitted. Most air being taken in passes through the face mask and is thus filtered, removing most or all virus particles. Ideally, respirators should be disposed of after each use, however, under certain conditions, they can be reused by the same person. These respirators should not be used when it is crushed, torn or creased, soiled or splashed with potentially infectious secretions, wet – no matter which liquid it has been wet with or when it becomes difficult to breathe while wearing it.

Respirators may be reused, only if they are in short supply. They can be reused by the same person, not shared among different people. If properly cared for, respirators can last one week or more. It must not be cleaned. They should be stored in a clean and dry location when not in use. They may be wrapped with a dry cloth or tissue. These should not be wrapped in plastic as this tends to retain moisture and reduce the face mask’s efficacy. Exposing used N95 masks to the right spectrum of UVC can help sanitise the mask in between use [6, 7].
Silicone masks
Silicone masks, which was developed by a research team at Massachusetts Institute of Technology (MIT) and Brigham and Women’s Hospital in Boston, are comparable to the performance of N95 masks and can also be sterilized and reused extensively. They can be autoclaved and cleaned using dry or steam sterilization and can be disinfected using alcohol and wipes. Although the designed mask fits criteria from the National Institute for Occupational Safety and Health (NIOSH), it is still under the process of finding a scalable solution [11].
Face shields
A face shield, an item of personal protective equipment protects the wearer’s entire face from hazards, chemical splashes, or potentially infectious materials. These are excellent at preventing droplets from coming into contact with the mouth, nose, and eyes but there are still high chances of inhaling droplets in the environment through the open areas around the plastic visor. Face shields work best to protect the wearer from an infected person when used with a mask [15].
Key issues and concerns
As vaccine is being rolled out, people are still advised to cover their nose and mouth while roaming around in public. As donning of face masks has proven to be important to help curb COVID-19, other barriers like social distancing, personal hygiene can also help in creating a combined effective method to reduce the spread and chances of getting infected as can be shown in Figure 6
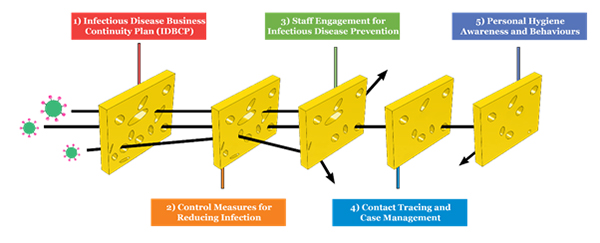
Figure 6. The Swiss cheese model showing various layers to prevent infectious diseases and control transmission risks
Correct methods on how to use masks and strict control by the governments not only on wearing masks but also on how they should be worn and handled can further reduce the spread of COVID-19. The Public must be trained about the correct way of putting on, wearing, removing, and disposing of face masks for face masks to be effective [12].
The COVID-19 aerosol, mainly appearing in the submicron region (d p between 0.25 and 1.0 μm) and super micron region (d p > 2.5 μm), can be effectively filtered out from the inhaled air by either surgical masks or N95 masks. A recent COVID-19 dynamic modelling study also suggested that broad adoption of even relatively ineffective non-medical grade “social” masks may meaningfully reduce the community transmission and decrease peak hospitalizations and deaths during the current COVID-19 pandemic [13].
A study conducted on the effectiveness of homemade masks as an alternative to commercial masks concluded that surgical masks are more effective in preventing microorganisms than homemade masks. Nevertheless, in short of supply scenarios, homemade cloth masks are better than no protection and 100% cotton is the best material to use while making them. The use of double-layer cotton masks reduces the emission of larger particles [14,16].
While utilizing cloth masks, care must be taken while removing and cleaning the masks as cloth masks can be prone to shedding fibres and in turn lodge deposited micro-organisms [16]. Few tips for cloth masks are shown in Figure 7.

Figure 7: Good practices while using facemasks [2]
Facemasks have always been a debatable topic as to its efficiency in controlling the pandemic. One should understand that wearing facemask only does not completely stop the virus, but at least acts as a layer of protection as mentioned earlier. Majority of the countries have adopted to implement mandatory face masking in public and on the other hand, there are countries which still haven’t. Countries with minority of residents wearing masks quickly contained outbreaks, but others had high death tolls. Places such as Denmark, Finland and Norway initially had their covid outbreaks controlled, but Sweden suffered high death toll rate at a later stage. As acknowledged by WHO, a reduction in infection rate by 85% was observed when masked.
All in all, a momentum has been observed in wearing facemasks as countries try and reopen their economics with covid still at bay. Facemasks have become a social behaviour, more or less like a car seatbelt. It will only prevent you from getting into a serious accident. Governments should proactively advise their population to wear facemasks as a layer of protection to effectively battle novel coronavirus and its emerging strains [20].
Precautions in wearing face masks
While wearing a face mask is essential, wearing them with proper precautions is also important. The effectiveness of face masks can be reduced if not wearing properly causing leakage or exposure of nose/ mouth to environment. This can be due to:
- Improper fitting
- Improper wearing
- Wearing old and worn out mask
- Wrong size
- Using or improper handling of contaminated mask
- Defective masks
- Bad behaviour when wearing mask (e.g., touch nose with hand)
- Etc.
The following precautions should be observed while wearing a face mask
- Hands should be properly cleaned with soap and water or hand sanitizer before touching the mask.
- Mask should be checked for any tears or holes before being used.
- The coloured side of the mask is usually in the front and away from the face while the white side faces towards the face.
- Hands should be thoroughly cleaned before and after the process of removing the mask. Touching the front face of the mask should be avoided.
- Mask should be properly discarded in the trash.
Environmental Concern on waste
Used Masks and Environment Issues
While the use of face masks as a first line of defence has been recognized, it is estimated that 129 billion masks are used and disposed of every month. That translates into 3 million face masks used per minute.
A separate study reports that 3.4 billion face masks or face shields are discarded every day. Asia is projected to throw away 1.8 billion face masks daily, the highest quantity of any continent globally. China alone, with the world’s largest population (1.4 billion) discards nearly 702 million face masks daily.
Face masks are made from multiple plastic fibers, primarily polypropylene, that will remain in the environment for decades, possibly centuries, fragmenting into smaller and smaller microplastics and nano plastics. A single face mask can release as many as 173,000 microfibers per day into the seas, according to a study in Environmental Advances.
Currently, most municipal systems do not allow for recycling of used masks. Masks can contain a mix of paper and polymers, including polypropylene and polyester, that can’t be separated into pure streams of single materials easily for recycling. They are also so small they get caught in recycling machinery, causing mechanical breakdowns.
The issue of used masks has arrived at a complicated time in the global effort to curb plastic waste. The amount of plastic waste accumulating in the oceans is originally forecast to triple in the next 20 years with no real solution on the horizon. This estimation was without the surge of plastic due to used masks. If every corporate pledge to use more recycled plastics were kept, the shift would reduce that projected tripling by just 7 percent (Parker 2021).
Can Reusable Masks Help
Even with reusable masks, their specific design and how you choose to clean them makes a difference. The University College London team examined the manufacture, use and disposal of masks that were disposable, reusable, and reusable with disposable filters, to calculate their overall environmental impact. They found machine washing reusable masks with no filters had the lowest impact over a year duration.
Hand washing masks increased the environmental impact due to machine washing uses electricity, but manual washing uses more water and detergent for each mask. Disposable filters also increase the environmental impact because the small filters are often made from plastic similar to the disposable masks, with a filter discarded periodically or after every use.
Perhaps surprisingly, the working paper estimates that hand washing reusable masks with disposable filters had the highest environmental impact overall – higher even than using fully disposable masks (Ketchell 2020).
What should be done
With all the above in mind, one should consider the following steps to reduce the impact of wearing a face mask:
- Use reusable masks without any disposable filters. Machine wash them regularly following the instructions for the fabric (assuming could achieve the desirable filtration one desired)
- Try to carry a spare so if something goes wrong with the one you’re wearing you don’t need to use or buy a disposable mask.
- If you do need to use a disposable mask, take it home (maybe in a bag if you have to take it off) and then put it straight into a bin with a lid. If this isn’t possible, place it in a proper public bin.
- Don’t put disposable masks in the recycling. They can get caught in specialist recycling equipment and be a potential biohazard to waste workers.
Section 5 References
- Tang, J. W., Noakes, C. J., Nielsen, P. V., Eames, I., Nicolle, A., Li, Y., & Settles, G. S. (2011). Observing and quantifying airflows in the infection control of aerosol-and airborne-transmitted diseases: an overview of approaches. Journal of Hospital Infection, 77(3), 213-222.
- WHO – Use of facemasks
- Wei, J., & Li, Y. (2016). Airborne spread of infectious agents in the indoor environment. American journal of infection control, 44(9), S102-S108.
- Kai, D., Goldstein, G. P., Morgunov, A., Nangalia, V., & Rotkirch, A. (2020). Universal masking is urgent in the COVID-19 pandemic: Seir and agent-based models, empirical validation, policy recommendations. arXiv preprint arXiv:2004.13553
- Schünemann, H. J., Akl, E. A., Chou, R., Chu, D. K., Loeb, M., Lotfi, T., ... & Mertz, D. (2020). Use of facemasks during the COVID-19 pandemic. The Lancet Respiratory Medicine, 8(10), 954-955
- Godoy, L. R. G., Jones, A. E., Anderson, T. N., Fisher, C. L., Seeley, K. M., Beeson, E. A., ... & Sullivan, P. D. (2020). Facial protection for healthcare workers during pandemics: a scoping review. BMJ global health, 5(5), e002553.
- Chughtai, A. A., Seale, H., & Macintyre, C. R. (2020). Effectiveness of cloth masks for protection against severe acute respiratory syndrome coronavirus 2. Emerging infectious diseases, 26(10).
- "Transmission-Based Precautions". U.S. Centers for Disease Control and Prevention. 2016-01-07. Retrieved 2020-03-31.
- Guidance on the use of masks to control influenza transmission.
- Engineers design a reusable alternative to N95 face mask.
- Jefferson, T., Foxlee, R., Del Mar, C., Dooley, L., Ferroni, E., Hewak, B., ... & Rivetti, A. (2008). Physical interventions to interrupt or reduce the spread of respiratory viruses: systematic review. Bmj, 336(7635), 77-80.
- Cumbo, E., & Scardina, G. A. (2020). Management and use of filter masks in the “none-medical” population during the COVID-19 period. Safety Science, 104997
- Davies, A., Thompson, K. A., Giri, K., Kafatos, G., Walker, J., & Bennett, A. (2013). Testing the efficacy of homemade masks: would they protect in an influenza pandemic?. Disaster medicine and public health preparedness, 7(4), 413-418.
- Why plastic face shields aren’t a safe alternative to cloth masks.
- Asadi, S., Cappa, C. D., Barreda, S., Wexler, A. S., Bouvier, N. M., & Ristenpart, W. D. (2020). Efficacy of masks and face coverings in controlling outward aerosol particle emission from expiratory activities. Scientific Reports, 10(1), 1-13.
- A user’s guide to masks: What’s best at protecting others and yourself. https://www.npr.org/sections/goatsandsoda/2020/07/01/880621610/a-users-guide-to-masks-what-s-best-at-protecting-others-and-yourself?t=1603376612321.
- Mantzari, E., Rubin, G. J., & Marteau, T. M. (2020). Is risk compensation threatening public health in the COVID-19 pandemic?. BMJ, 370.
- Coronavirus is not cancelled: Wear your mask.
- Coronavirus: Which Countries Have Mask Mandates and Do They Work? (bloomberg.com)
- BSI-guide-to-PPE-masks.pdf (eda.org.uk)
- Laura Parker (15 April 2021). How to stop discarded face masks from polluting the planet. National Geographic
- Misha Ketchell (15 August 2020). Coronavirus face masks: an environmental disaster that might last generations. The Conversation.